Executive summary
Assisted reproductive technologies (ART) have revolutionized reproductive medicine, offering hope to millions facing fertility problems through methods like artificial insemination to cutting-edge gene editing. While established techniques such as in vitro fertilization and intracytoplasmic sperm injection are widely used today, emerging technologies such as in vitro gametogenesis, gene therapies, and stem cell-based therapies are expanding the boundaries of what is possible.
ART is a rapidly advancing field, but the use of certain novel and emerging technologies in humans is still highly experimental, tightly regulated, and surrounded by ethical and legal challenges. Many innovations in ART are being tested only on animal models, yet some have successfully transitioned to human applications, including preimplantation genetic testing, mitochondrial replacement therapy, time-lapse imaging, and in vitro maturation. Furthermore, artificial intelligence is transforming reproductive medicine by enabling precise embryo selection, optimizing clinical protocols, and predicting treatment outcomes.
This report explores data from the CAS Content CollectionTM to outline the research progress in ART and identify key emerging concepts and challenges to better understand how ART is shaping the future of reproductive healthcare.
State of the ART: An introduction
Assisted reproductive technology (ART) encompasses a broad spectrum of medical techniques designed to aid individuals and couples in overcoming infertility challenges and enabling child conception. Infertility affects approximately 10-15% of couples worldwide, making ART a critical component of modern healthcare.
ART procedures typically involve the handling of eggs, sperm, and embryos to achieve fertilization and implantation. Techniques such as IVF and cryopreservation are now standard practices in fertility clinics worldwide. In recent years, emerging technologies like artificial intelligence (AI), genetic testing, and stem cell research have further refined ART, enhancing its success rates while addressing ethical and social implications. Furthermore, experimental innovations like in vitro gametogenesis (IVG) could provide gametes for individuals who are unable to produce their own.
Yet many ethical questions remain around various ART innovations, and many still rely heavily on animal models. This approach provides valuable insights into reproductive biology and the effects of various ART interventions, but it shows that many innovations are still far from clinical usage in humans.
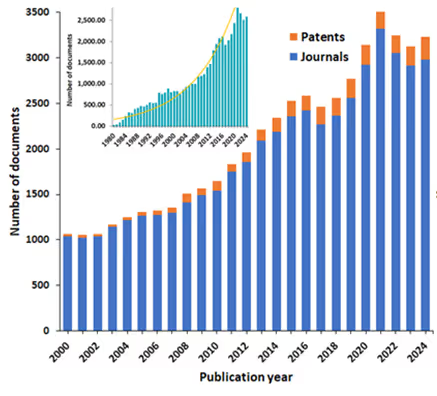
We explored data from the CAS Content CollectionTM, the largest human-curated repository of scientific information, to outline research progress in ART. The growth in publications since the year 2000 demonstrates the widespread research and commercial interest in these innovations with the number of ART-related publications tripling in the last two decades (see Figure 1).
Current methods of assisted reproductive technology
Efforts to overcome infertility have a long history, starting with the first documented case of artificial insemination in 1790. The first pregnancy achieved through in vitro fertilization of a human oocyte happened in 1973, although it ended in miscarriage. In 1978, the first successful IVF pregnancy and live birth took place, and by the 1980s, IVF had become mainstream.
Over 8 million babies have been born with IVF, and ART methods are now well-established parts of reproductive medicine worldwide. The most common traditional methods include:
- IVF is a cornerstone of human fertility treatment, enabling millions of births worldwide. IVF includes ovarian stimulation using fertility drugs to produce multiple eggs, retrieval of mature eggs through a minor surgical procedure, fertilization of eggs with sperm in a laboratory dish, and transfer of resulting embryos into the uterus. Currently fully integrated into clinical practice, it is successfully applied in tubal factor infertility, endometriosis, male factor infertility, and unexplained infertility. Success rates vary by age, with the highest success rates (30-40% per cycle) for women under 35. In our analysis of the CAS Content Collection, we found that IVF constitutes the largest portion of ART-related documents (see Figure 2).
- Artificial insemination is a medical procedure in which sperm is introduced into a woman's reproductive tract to facilitate fertilization and pregnancy. A sperm sample is collected, washed and concentrated to isolate healthy sperm, then placed directly into the uterus (intrauterine insemination, IUI) or cervix (intracervical insemination, ICI) during ovulation. It is mainly applied in cases of mild male infertility, unexplained infertility, or cervical mucus issues. It is simpler and less invasive than IVF. Success rates are typically 10-20% per cycle, depending on factors like age and sperm quality.
- Gamete intrafallopian transfer (GIFT) is a procedure that helps women conceive by placing eggs and sperm directly into the fallopian tubes. Eggs and sperm are collected and mixed before being placed into the fallopian tube via laparoscopy, allowing fertilization to occur naturally in the body. This method is less common today due to advances in IVF.
- Zygote intrafallopian transfer (ZIFT) is like IVF, but the fertilized egg (zygote) is transferred into the fallopian tube instead of the uterus. It is applied to infertile patients with healthy fallopian tubes. It combines the benefits of IVF and GIFT but is less common now.
- Cryopreservation (fertility preservation) involves freezing and storing reproductive cells, such as eggs, sperm, or embryos, for future use. Cryopreservation is now a routine procedure for embryos and sperm and is becoming more common for oocytes. It is applied for fertility preservation, e.g., for cancer patients undergoing chemotherapy or radiation therapy, excess embryos from IVF, or those delaying childbearing for personal or professional reasons.
- Egg donation and sperm donation can help people have children when they are unable to produce healthy eggs or sperm on their own. Eggs or sperm are donated by a third party and used in ART procedures like IVF or intrauterine insemination to achieve pregnancy. This method is widely used by older women, same-sex couples, or single parents.
- Surrogacy involves a woman carrying and giving birth to a child for another person or couple using their embryos (gestational surrogacy) or her own egg (traditional surrogacy). While in traditional surrogacy the surrogate’s egg is fertilized with sperm (via IUI or IVF), making her the biological mother, in gestational surrogacy, the surrogate carries an embryo created through IVF using the intended parents’ or donors’ eggs and sperm, so she has no genetic link to the child.

Fastest-growing ART methods: AI and in vitro gametogenesis
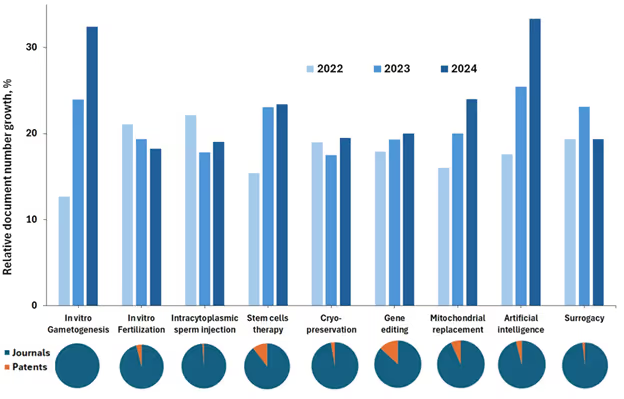
Traditional ART methods have been groundbreaking, but they have many drawbacks, including high costs, physical and emotional stress, health risks, and ethical and legal issues. New innovations are offering greater hope for people struggling with infertility, and our analysis of the CAS Content Collection shows that the use of AI in ART and in vitro gametogenesis (IVG) are the fastest growing novel methods in the last three years (2022-2024) (see Figure 3).
AI in ART
For embryo selection, AI algorithms analyze embryo images to assess their quality and potential for successful implantation. These algorithms use:
- Time-lapse imaging: AI monitors embryo development over time, evaluating factors such as morphology, cell division patterns, and dynamics.
- Morphokinetic data: algorithms predict the likelihood of an embryo developing into a viable pregnancy by identifying subtle features not visible to the human eye.
AI also helps improve sperm selection by identifying the most motile and morphologically normal sperm and through DNA integrity checks, which assess DNA fragmentation levels in sperm to select the healthiest candidates.
Machine learning models analyze multiple data points to predict the success rate of IVF, including patient history (age, hormonal levels, lifestyle factors), clinical data (ovarian reserve markers, endometrial receptivity), and embryo quality metrics. AI can optimize ovarian stimulation protocols by personalizing medication dosages based on patient-specific responses and predicting ovarian responses to stimulation, reducing the risk of ovarian hyperstimulation syndrome (OHSS). Identifying the optimal timing for clinical interventions such as egg retrieval and embryo transfer are critical to the success of ART cycles, and researchers have seen notable improvements with AI-driven models.
Our analysis revealed an increase of patents relating to AI-driven innovations, such as a patent assigned to Cornell University in 2025 that uses machine and/or deep learning to analyze and predict the ploidy status of an embryo. Univfy also recently patented computer-aided methods of assessing the probability of a patient having an IVF failure or an intermediate treatment outcome.
AI-driven automation streamlines processes in ART labs, including monitoring and controlling incubator conditions, standardizing embryo grading to minimize human error, and managing cryopreservation protocols. By leveraging large datasets from clinics and research studies to identify trends and factors influencing ART success, AI can recognize patterns in patient and embryo data and improve treatment protocols. Thus, the uses of AI in ART are extensive and could provide improved outcomes for many patients.
IVG in ART
IVG is an experimental technology that enables the creation of sperm or eggs from somatic cells, such as skin or blood cells. IVG involves the differentiation of pluripotent stem cells (PSCs) like embryonic stem cells (ESCs) or induced pluripotent stem cells (iPSCs) into gametes. This process mimics the natural progression of gametogenesis, where primordial germ cells develop into mature gametes through intricate molecular and cellular pathways. What makes it exciting is that it could provide gametes for those unable to produce viable eggs or sperm.
Researchers have successfully produced functional gametes in animal models including mice, leading to healthy offspring. However, translating these techniques to human systems remains a work in progress due to the complexity of human gametogenesis and important ethical concerns. In 2024, scientists at Kyoto University created precursors to human gametes from induced pluripotent stem cells (iPSCs), but significant hurdles remain before this technique can be widely used.
Despite the recent breakthroughs in IVG, ethical concerns remain. Embryo creation and manipulation, namely creating and discarding large numbers of embryos, must be addressed before implementation. Safety and efficacy also require extensive validation before clinical application.
Methods of greatest commercial interest: Stem-cell therapies and gene editing
As seen in the pie charts at the bottom of Figure 3, gene editing and stem cell-based therapies have the highest patent fraction of all documents (13% and 10%, respectively), which is indicative of high commercial interest.
Stem cell-based therapies
Stem cells can differentiate into reproductive cell types, such as embryonic stem cells or induced pluripotent stem cells to form oocytes or sperm; they secrete paracrine signals that enhance tissue repair and cellular function; and they can integrate into reproductive tissues, contributing to structural and functional recovery.
The application of stem cell-based therapies in ART could drive numerous breakthroughs:
- Age-related decline in ovarian reserve is a major cause of infertility. Mesenchymal stem cells and bone marrow-derived stem cells have shown promise in regenerating ovarian tissue, improving folliculogenesis, and restoring hormonal balance.
- Stem cell transplantation has demonstrated potential in restoring spermatogenesis in individuals with azoospermia or other forms of male infertility. Spermatogonial stem cells (SSCs) can be harvested, cultured, and reintroduced into the testes to reinitiate sperm production.
- Conditions such as Asherman’s syndrome and thin endometrium pose significant challenges for successful implantation. Endometrial stem cells (ESCs) and MSCs have been explored to regenerate and enhance endometrial receptivity.
- As noted, deriving gametes (eggs and sperm) from pluripotent stem cells via IVG opens new possibilities for biological parenthood.
Various stem cell types used in ART are summarized In Table 1.
Table 1: Stem cell types in ART.
Gene editing
Gene editing in ART has the potential to reduce heritable disorders, improve embryo selection, and enhance reproductive success rates. It can correct mutations in embryos associated with hereditary diseases such as cystic fibrosis, sickle cell anemia, and Huntington's disease, preventing their transmission to future generations. Another application of gene editing in ART is the enhancement of embryo selection — genetic screening combined with editing can improve embryo quality by selecting embryos with the highest potential for successful implantation and development. Gene editing can also help address infertility by identifying and correcting genetic causes of infertility, such as chromosomal abnormalities or mutations affecting gamete function.
The CRISPR-Cas9 system is the most prominent tool in gene editing. By targeting specific DNA sequences, CRISPR-Cas9 can add, delete, or alter genes, making it a valuable technology in addressing inherited genetic disorders in embryos created via IVF.
However, this technique is controversial due to the potential for "designer babies" and unintended consequences. Currently, gene editing in humans, particularly germline editing, which affects eggs, sperm, or embryos and can be passed on to future generations, is heavily restricted or banned in many countries due the concerns.
Some notable patents have been assigned in this field recently; for example, Fujita Academy received a patent in 2024 for a method of testing chromosomal aneuploidy of embryos using non-coding RNA for infertility treatment. This process tests embryos cultured in vitro and creates an extracellular RNA profile by performing machine learning and determining the presence or absence of chromosomal aneuploidy.
Additional novel methods in ART
Our analysis of the CAS Content Collection reveals several other novel methods that are gaining traction in ART:
Genetic screening
One of the most significant trends in ART is the integration of advanced genetic screening techniques. Preimplantation genetic testing (PGT) has become increasingly sophisticated, allowing for the detection of chromosomal abnormalities and single-gene disorders in embryos before implantation.
- PGT-A (aneuploidy screening) technique screens for chromosomal abnormalities, which are a leading cause of implantation failure and miscarriage. Advances in next-generation sequencing (NGS) have improved the accuracy and efficiency of PGT-A, leading to higher success rates in IVF cycles.
- PGT-M (monogenic disorders) is used to identify embryos carrying specific genetic mutations, enabling couples with hereditary conditions to have healthy offspring. The development of CRISPR-Cas9 and other gene-editing tools has further enhanced the potential for correcting genetic defects at the embryonic stage.
- PGT-SR (structural rearrangements) testing is designed for individuals with chromosomal translocations or inversions, helping to identify embryos with balanced chromosomal structures.
These advancements not only improve the likelihood of a successful pregnancy but also reduce the risk of passing on genetic disorders, offering a more personalized approach to reproductive medicine.
Mitochondrial replacement therapies
Mitochondrial replacement therapy (MRT), also known as mitochondrial donation, is a technique that aims to prevent the transmission of mitochondrial DNA (mtDNA) disorders from mother to child. This involves replacing defective mitochondria in an egg or embryo with healthy mitochondria from a donor.
MRT has been used to create embryos with genetic material from three individuals: the mother, the father, and a mitochondrial donor (so called “three-parent babies”). MRT raises ethical concerns related to genetic modification and the long-term effects on future generations. However, this procedure is beneficial for women with mitochondrial disorders who wish to have genetically related children. The technology is currently regulated differently across countries, with some permitting its use under strict guidelines and others banning it.
There are certain key differences between MRT and gene editing, as outlined in Table 2:
Intracytoplasmic sperm injection (ICSI)
ICSI is an ART procedure that involves injecting live sperm directly into the cytoplasm of a mature egg using a micromanipulation tool. The fertilized egg is then cultured and transferred as in IVF. It represents a refinement of IVF and is the most common and successful treatment for male infertility caused by sperm issues, such as low sperm count, poor motility, or abnormal morphology, or when previous IVF attempts have failed. Success rates are similar to IVF, but ICSI can significantly improve fertilization rates in cases of male infertility.
Improved embryo culture systems
There are many ways to improve embryo culture systems, including a new type of culture platform design which creates a better microenvironment for embryos. New media formulations including antioxidants to reduce oxidative damage and improve blastocyst development are also being researched, as are perfusion-based systems using dynamic media flow instead of static culture.
Advances in time-lapse imaging and optimized culture media also allow for continuous monitoring of embryo development, enabling better selection for transfer and increasing implantation rates.
Cryopreservation enhancements
Cryopreservation techniques in ART have improved in several ways including vitrification, which is a rapid freezing process that prevents ice crystal formation, thereby improving survival rates of frozen gametes and embryos. Researchers are also developing improved and optimized cryoprotectants; for example, vapor tanks storing tissue in the vapor phase of nitrogen instead of immersing it in liquid nitrogen offers better survival rates for frozen eggs, sperm, and embryos.
Fertility preservation innovations
Techniques such as ovarian tissue cryopreservation and artificial ovary development are advancing, benefiting individuals facing fertility-impacting medical treatments. The ovarian rejuvenation technique is used to stimulate the ovaries to produce new eggs, particularly in women with diminished ovarian reserve or premature ovarian failure. It may include injecting platelet-rich plasma (PRP) into the ovaries to stimulate tissue repair and egg production, or stem cells to regenerate ovarian tissue. The technique is still experimental with mixed results in early studies.
Non-invasive and automated technologies
Time-lapse imaging, the continuous monitoring of embryos without the need for manual handling, improves embryo selection and reduces stress on the embryos. Automated IVF systems are being integrated into laboratories to improve the efficiency and consistency of processes like fertilization and embryo transfer. Non-invasive forms of genetic testing to assess the genetic health of embryos, such as the use of culture media rather than invasive biopsy, are being developed to minimize risks.
Artificial wombs
Research into ectogenesis, or artificial womb technology, aims to support the development of embryos outside the human body. Such technology provides solutions for individuals unable to carry pregnancies due to medical or anatomical reasons and advances neonatal care by supporting extremely premature infants.
ART research in animal models
Because many ART methods raise ethical and legal concerns, researchers must rely on animal models to develop and optimize these techniques. Animal models are indispensable in ART research due to their biological and physiological similarities to humans and their role in studying species-specific reproductive processes. Moreover, they provide a controlled environment to study the mechanisms of reproduction, test new technologies, and assess the safety and efficacy of ART interventions.
Common animal models in ART research include:
- Rodents (mice and rats) due to their short reproductive cycles, ease of genetic manipulation, and low cost.
- Livestock (cattle, sheep, and goats), which can contribute to agricultural efficiency and wildlife conservation by adapting techniques for endangered species.
- Non-human primates because they are the closest models to humans in reproductive biology.
- Zebrafish, which have a unique model for early embryogenesis due to their external fertilization and transparent embryos.
- Wildlife models that assist global conservation efforts by enhancing genetic diversity and population recovery.
Animal models remain indispensable in ART research, serving as a bridge to ensure that human applications are safe and effective. In Table 3, we compare techniques used in animal models and humans:
Challenges and ethical considerations
While ART methodologies hold immense promise, they present unique challenges and ethical considerations. Safety must also be considered since the long-term effects of many procedures are still unknown. As a result, there are numerous areas of concern around implementing these innovations:
- Embryo-related ethics: Creating more embryos than needed raises concerns about what happens to unused embryos. Some view the disposal of embryos as ethically problematic.
- Parental and child rights: Use of egg and sperm donors and surrogates introduces legal and emotional complexities regarding parental rights and the child’s right to know their genetic origins. Using gametes or embryos from deceased individuals raises questions about consent and the welfare of the resulting child. Societal biases and legal hurdles may affect the access of same-sex couples or single individuals to ART.
- Legal and regulatory issues: ART practices and laws vary across countries, leading to ethical inconsistencies. People traveling to countries with more lenient ART laws may exploit loopholes, complicating ethical oversight and enforcement. The use of AI and genetic data in ART also raises concerns about patient confidentiality and potential misuse of sensitive information.
Perhaps the most complicated issues surround genetic and technological ethics. Technologies like CRISPR used in ART raise concerns about unintended consequences, heritable changes, and societal implications of altering human genetics. Indeed, changes made to germline cells are heritable, meaning they affect future generations. This generates ethical questions because future generations cannot consent to these modifications.
There are fears that gene editing could be used for non-therapeutic enhancements (e.g., selecting for intelligence, appearance, or athletic ability), leading to societal inequality and eugenics-like practices. Also, some groups argue that altering human DNA is "playing God" or interferes with natural processes.
Safety concerns must also be addressed before ART innovations can be widely used in clinical settings. Once again, there are concerns about gene editing due to the lack of sufficient data on long-term consequences and possible off-target effects. Unintended mutations could have serious consequences for individuals and future generations, making it crucial to fully understand the potential long-term effects before clinical application. Even precise gene editing tools like CRISPR can sometimes make edits at unintended locations in the genome ("off-target effects"), which could lead to unforeseen health complications.
Regulatory agencies are engaging with the scientific community to establish frameworks for the safe and ethical use of gene-editing technologies. There is a rising urgency to involve the public in debates regarding the ethical, legal, and social implications of gene editing. The World Health Organization (WHO) has called for a global registry of human gene-editing research and stricter oversight, and the UNESCO International Bioethics Committee has recommended a moratorium on germline editing.
Various countries have different rules regarding ART. For example, in 2023, the UK approved CRISPR-based therapies for treating blood disorders like sickle cell anemia and beta-thalassemia, marking a significant step forward for somatic gene editing. Germline editing in the U.S. is not banned but is heavily restricted, and in many other countries including European nations and Australia, the practice is prohibited.
The future of ART
Emerging technologies in ART are pushing the boundaries of reproductive medicine, offering hope to individuals facing infertility while raising profound ethical and societal questions. From AI-driven embryo selection to in vitro gametogenesis and gene editing, these advancements promise to redefine parenthood.
However, translating these innovations into clinical practice requires careful consideration of safety, accessibility, and ethical implications to ensure equitable and responsible use. Once an ART innovation proves successful in animal models, it progresses to clinical trials in humans, beginning with small, carefully monitored studies. Innovations like time-lapse imaging and AI-driven embryo selection have all transitioned from theory or animal-based research to human use after rigorous validation.
The questions surrounding ART are complex, and science still has much to learn before more of these breakthroughs can be brought into clinical practice. However, as our analysis shows, innovative approaches to reproductive technologies are a beacon of hope and a testament to scientific ingenuity.