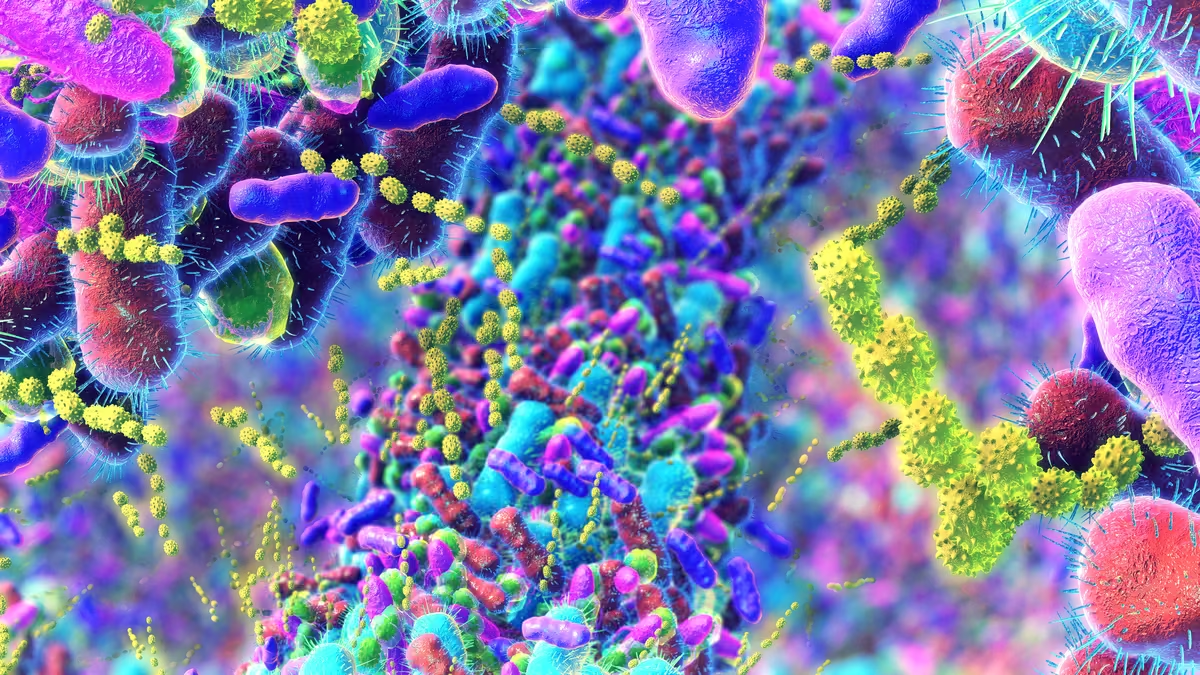
Emerging Science
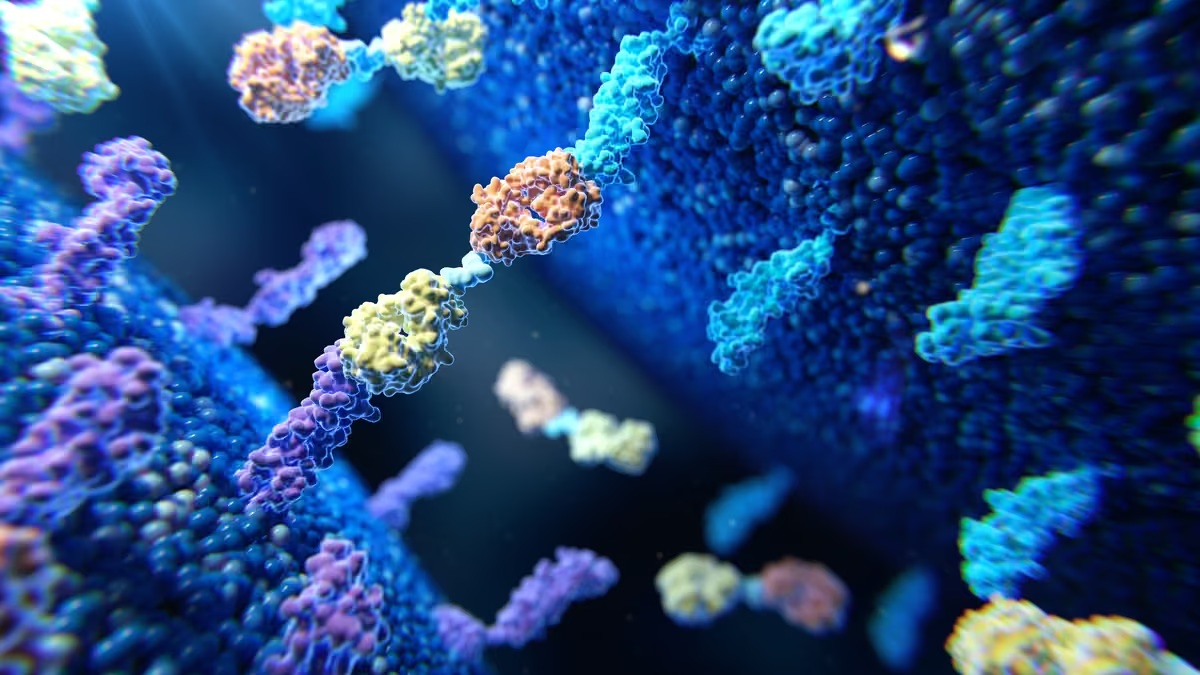
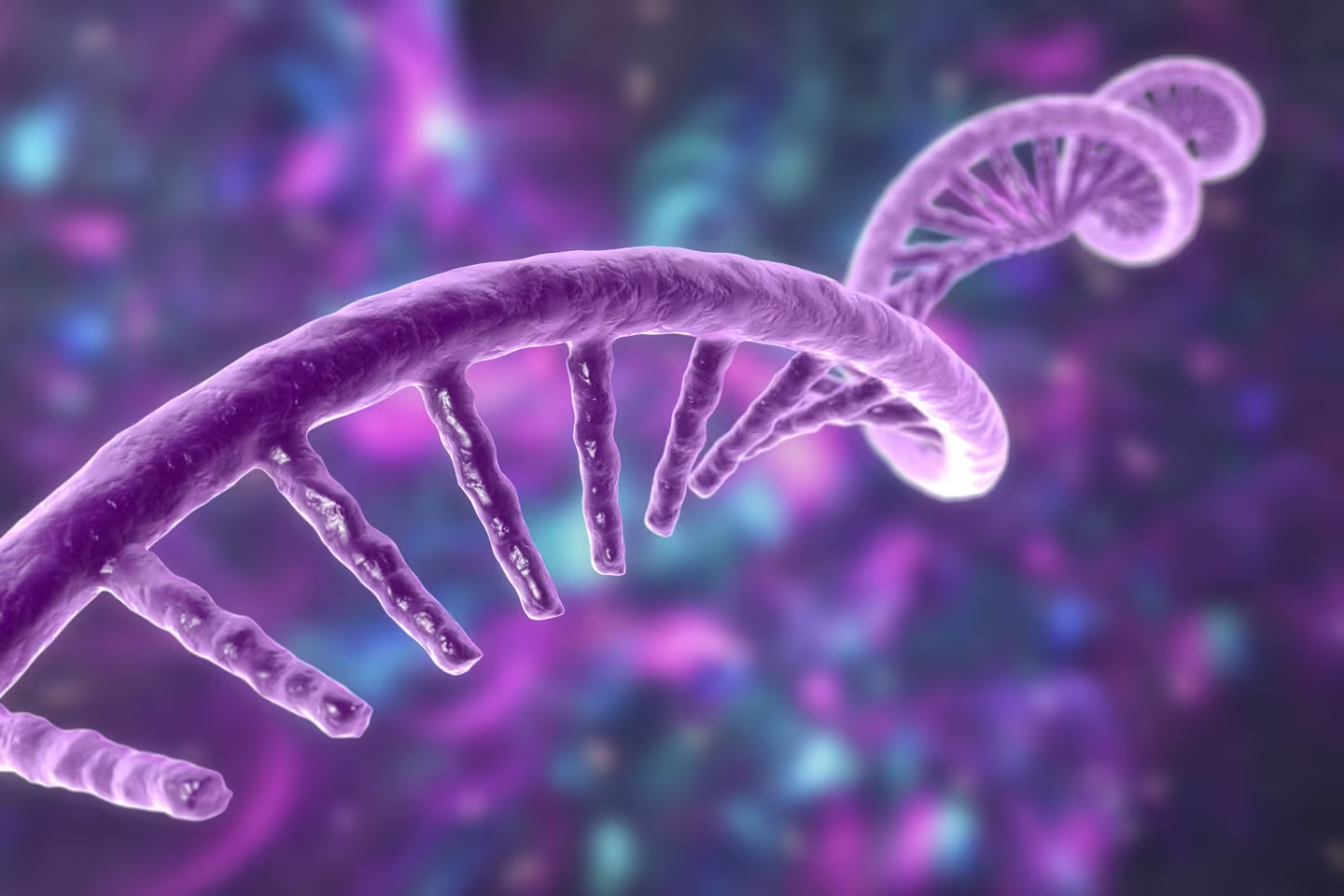
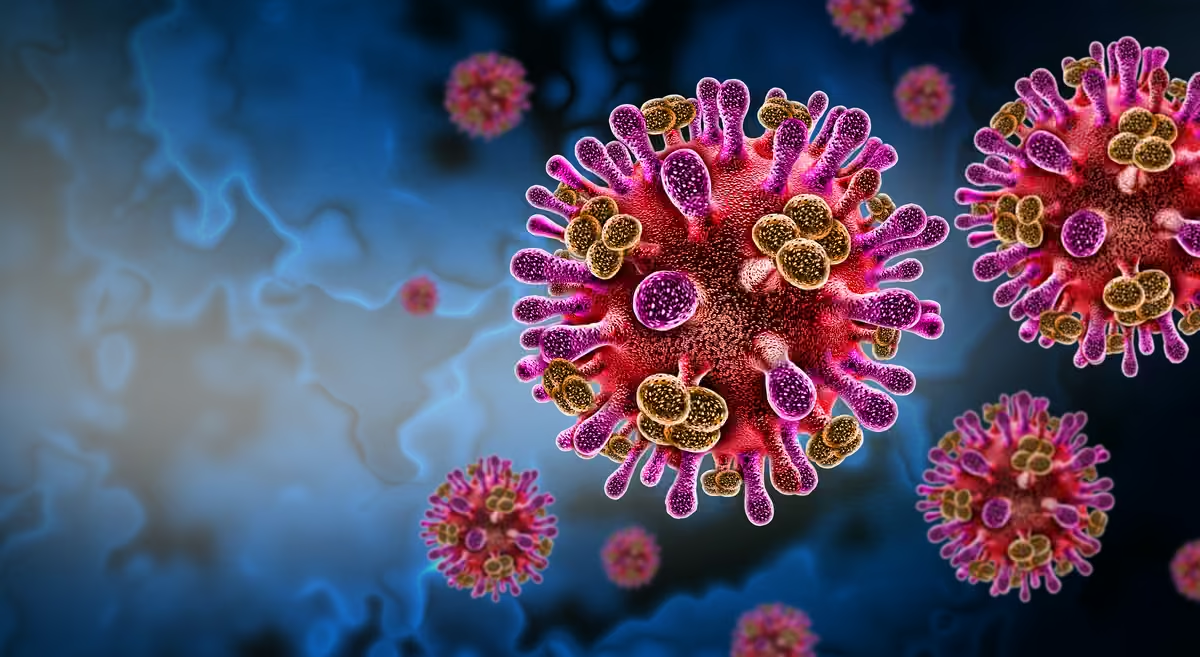
Nipah virus explained: Risks, realities, and the hope from new research
New Nipah cases in India have renewed focus on a high‑fatality zoonotic threat shaped by complex spillover dynamics, severe neurological disease, and limited medical countermeasures. Meanwhile, global efforts in diagonistcs, therapeutics, and vaccines are accelerating.
Read the reportRead the articleDownload the summarySee the infographicRead the publicationRead the recapWatch the video